Findings and Pathophysiology in left sided congestive heart failure
Radiographic signs of left-sided heart failure include left atrial enlargement, pulmonary venous engorgement, peribronchial pattern, and air bronchograms. The constellation of these findings provides compelling evidence of pulmonary edema.
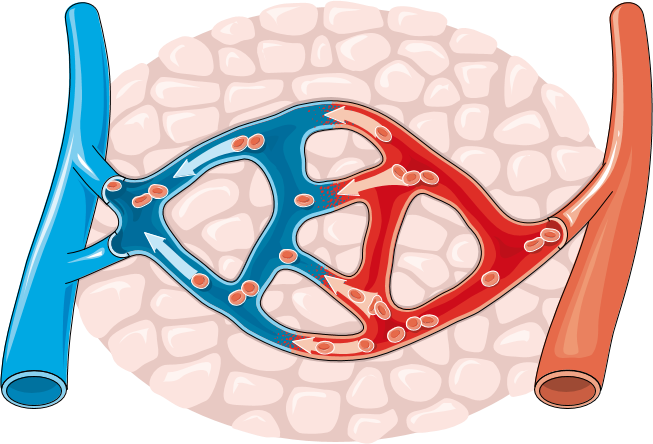
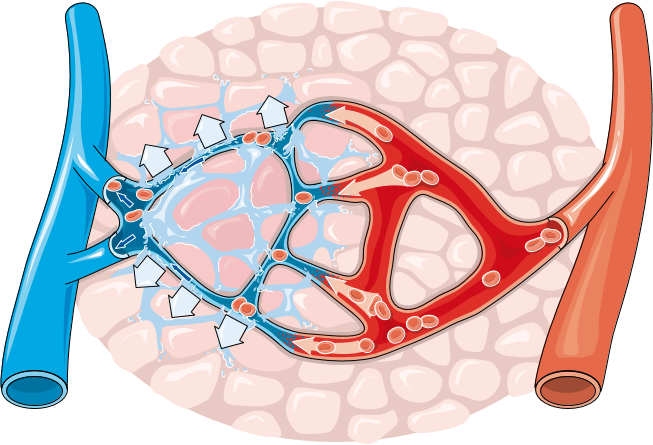
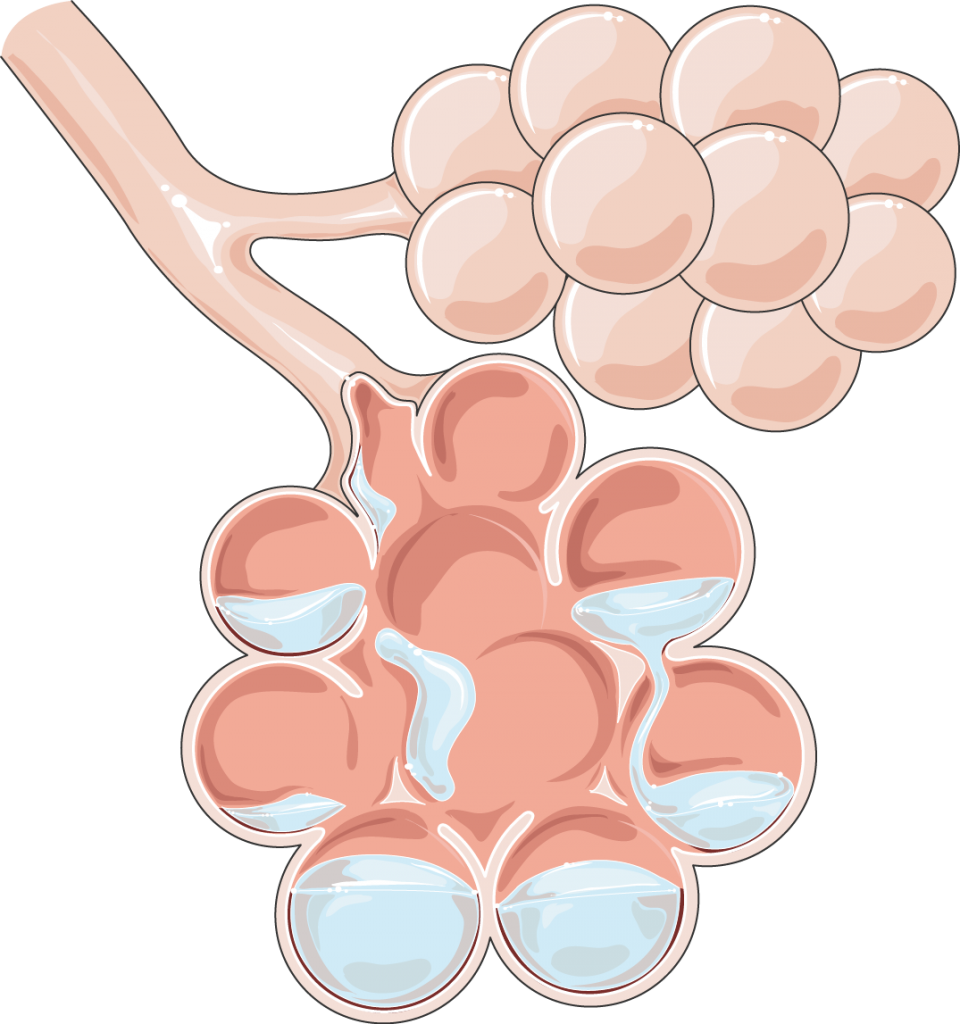
Left-sided heart failure occurs when the heart loses its ability to pump oxygenated blood to the rest of the body efficiently. This can result in the “backing up” of blood pressure from the left ventricle, to the left atrium, to the pulmonary veins and finally the pulmonary capillary beds. This elevated hydrostatic pressure in the pulmonary capillaries disturbs Starling Forces across the capillary membrane causing fluid to “leak” into the pulmonary interstitium resulting in edema. Radiographic signs of left sided heart failure therefore begin with evidence of pulmonary venous engorgement. As fluid “leaks” into the pulmonary interstitium it collects along the triad of artery, bronchus, and vein causing the so called “peribronchial pattern”, and silhouetting of the margins of the pulmonary arteries and veins. And finally, as fluid continues to “leak” into the interstitium it fills the alveoli causing the radiographic finding of “air bronchograms”. Patients often present with a history of exercise intolerance due to the reduced amount of oxygenated blood being pumped to the rest of the body by the left ventricle. Since fluid will be leaking out of the vasculature due to increased hydrostatic pressure, the patient may also have trouble breathing due to fluid in the lungs.
The increase in hydrostatic pressure results in the passage of fluid from the capillaries, through their loose junctions, into the surrounding interstitium. At this stage, peribronchial patterns would likely be detectable on radiographs.