Atrial Fibrillation
Atrial fibrillation is a supraventricular arrhythmia associated with many microfoci of atrial myocardium acting as ectopic foci or serving as small reentrant pathways and activating the adjacent atrial myocardium. Only the ectopic foci that manage to depolarize close to the A-V node successfully penetrate the A-V node to activate the ventricles. There is no coordinated atrial contraction, and the ventricles are activated at a fast rate and at irregular intervals.
ECG Findings:
- Typically rapid and always irregular ventricular rhythm.
- No distinct P waves; at times the baseline may show very fine baseline undulations which are called fibrillation waves. However sometimes these fibrillation waves are not apparent.
- The QRS complexes are supraventricular in origin thus the QRS complexes tend to look of normal morphology. They may be wide if there is underlying ventricular myocardial disease.
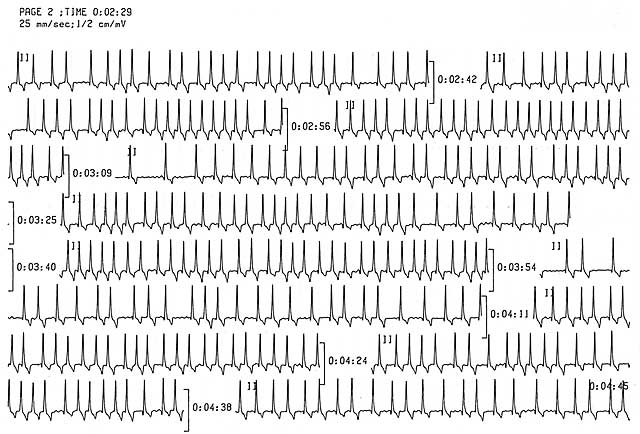
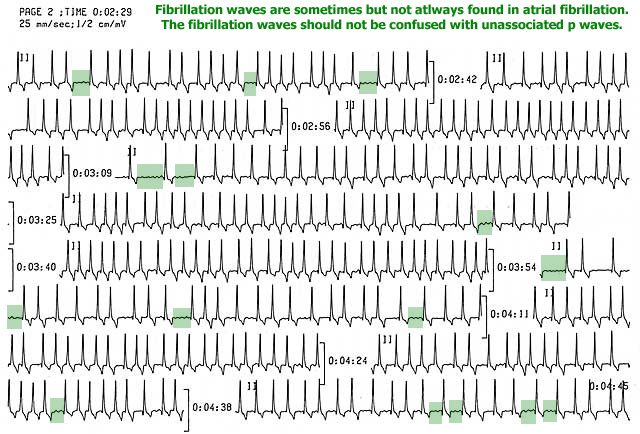
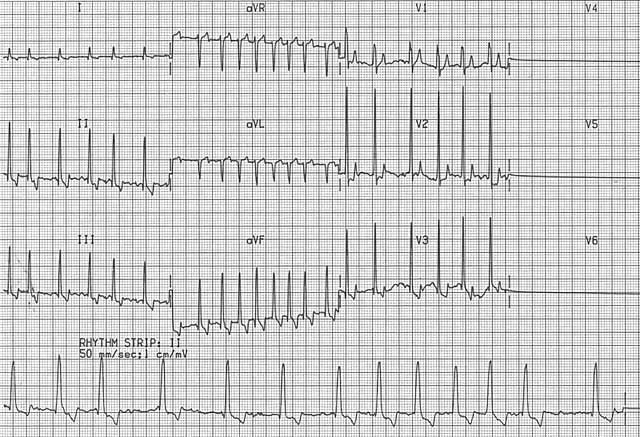
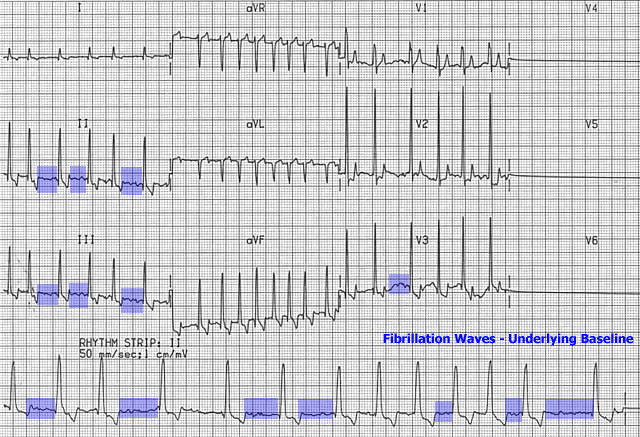
The hallmark ECG findings are the presence of an irregular rhythm and absence of P waves. As the heart rate becomes very rapid, the rhythm approaches a regular rhythm; however, a slight irregularity remains present. Although the heart rate is usually rapid, it can be slow if:
- A giant breed of dog is involved
- A-V nodal disease co-exists
- Medication such as digitalis, beta-blocker, or calcium channel blocker therapy is on board
Etiology:
- Due to a very high number of microfoci or small reentrant pathways in the atria. They are competing to activate the A-V node.
- Due to disorders associated with atrial dilation.
- A-V valvular insufficiency
- Cardiomyopathy
- Congenital heart disease
- May occur in the absence of organic heart disease (often giant breed dogs). These patients usually have slow to normal ventricular rates.
Consequence:
- The rapid ventricular rhythm results in a fall in cardiac output due to excessive heart rate.
- Cardiac output also falls due to a loss of atrial contraction. At rapid rates, the atrial component to ventricular filling can account for up to 30% of ventricular filling. At slower rates, the atria contribute relatively little to ventricular filling.
- The rapid heart rates also result in an increase in myocardial oxygen consumption. This can result in more myocardial hypoxia which causes a reduction in inotropy and exacerbation of dysrhythmias.
Treatment options:
- Convert the rhythm to a sinus rhythm
- Although direct current electrical cardioversion is possible, most individuals revert back to atrial fibrillation because of the underlying atrial pathology
- Slow the ventricular rate – reduce the tachycardic effect on cardiac output and the effect of loss of atrial filling
- Calcium channel blocker – diltiazem is often a drug of choice to slow the heart rate
- Beta blocker – e.g. propranolol, metoprolol, atenolol
- Digoxin
- Combination of diltiazem and digoxin – a study of 18 dogs with advanced cardiac disease and atrial fibrillation showed that better rate control was achieved with the combination of diltiazem and digoxin compared with either drug on its own (Gelzer et al. JVIM 2009;23:499-508).
- Amiodarone – not only may slow rate, but may result in conversion to sinus rhythm in some cases, however associated with a significant adverse side effect profile
